
Choosing pressure relief equipment
Choosing pressure relief equipment
This factsheet is available for sponsorship, email marketing@dlf.org.uk
Sponsorship has no influence on our impartial content
Contents
- Introduction
- Risk factors
- Who is at risk?
- Reducing the risk of pressure ulcers
- Properties and features of pressure relief mattresses and cushions
- Types of materials used in mattresses, overlays and cushions
- Advice for people who need pressure relief whilst sitting in an armchair
- Types of beds with pressure relieving features
- Joint protectors
- Supply and provision
- Permanent loan: health and local authority provision
- Home nursing equipment
- Employment service
- Purchase of equipment
- Home nursing equipment
- Selecting appropriate equipment
- Further advice from us
- Useful organisations
- References
Introduction
Pressure ulcers (which are often referred to as bedsores or pressure sores) are areas of damage to the skin and underlying tissue, usually occurring over bony prominences. They are caused by:
- pressure - occurs when skin and tissue are directly compressed between bone and a support surface such as a bed or wheelchair. Blood is unable to circulate causing a decrease of oxygen and nutrients to the underlying cells
- shear - occurs when skin and tissue are pulled in different directions, for example when a person slips down a bed or is repositioned using a dragging motion
- friction - occurs when the skin rubs against a surface, for example the heels rubbing against a sheet.
The greatest areas at risk are those where there are weight bearing bones near the surface of the skin, for example under the bones in the buttocks (the ischial tuberosities), the shoulders, hips and heels.
Both people at risk, and their carers, need to be aware of the importance of pressure ulcer prevention. Pressure ulcers can be painful, difficult to treat and even life threatening in extreme cases.
A prevention programme may include:
- regular skin assessment
- use of manual handling aids and techniques
- regular repositioning
- continence management
- the use of pressure distributing equipment.
For further information on prevention and treatment guidelines, refer to the Royal College of Nursing’s Pressure ulcer risk assessment and prevention or the European Pressure Ulcer Advisory Panel. The Medicines and Healthcare Products Regulatory Agency has completed assessments regarding many types of pressure relief equipment, see Useful Organisations below).
Risk factors
Several factors may increase a person’s risk of developing pressure ulcers:
Decreased mobility
People with decreased mobility may have difficulty relieving pressure when sitting or lying. As a result, they may be unable to reposition themselves in a chair or a bed, or may slip down in a chair, producing a shearing effect. When carers assist people to reposition or transfer from a chair or bed, inappropriate manual handling techniques may also cause shearing or friction.
Neurological impairment or sensory impairment
People with a neurological impairment or decreased sensation may not feel the uncomfortable sensation of pressure building up and therefore may be unable to reposition themselves in order to relieve pressure. These people may not even feel when a pressure ulcer has developed.
Incontinence
The inability to control the bladder and/or bowel increases dampness in the buttock and thigh area, making the skin more prone to damage. Further information about this can be found here. Advice and help can be sought from your GP or local continence service and information about this can be found on the NHS website.
Temperature and humidity
Increased heat and humidity can cause sweating which can add to the risk of skin breakdown. Skin cell function is also impaired if the skin becomes too warm or too cold, increasing the skin’s susceptibility to damage.
Decreased nutrition and circulation
People with low body fat may have decreased subcutaneous fat and muscle bulk, providing little padding over bony prominences. People with high body fat have increased padding over bony prominences, but this tissue is poorly vascularised and may be more prone to shear forces. Good nutrition is required to repair tissue and prevent ulcer occurrence, and good hydration is required to maintain the resistance and elasticity of the tissues.
Who is at risk?
In general, people who spend most of the day lying or sitting and are unable to reposition themselves effectively are at risk of developing pressure ulcers.
A number of risk assessment scales are designed to assist health professionals to identify a person at risk of developing pressure ulcers, including the Norton Scale and the Waterlow Scale.
When a pressure ulcer has developed, the ulcer is usually graded in the following way:
- Grade1 – reddened skin which persists for more than 30 minutes after pressure has been relieved
- Grade 2 – superficial skin damage. May present as a blister or as an abrasion
- Grade 3 – full thickness skin loss not extending to bone or muscle. This grade of pressure ulcer is not usually painful
- Grade 4 – full thickness skin loss with extensive tissue damage through to muscle and bone.
(NHS Choices 2017)
Reducing the risk of pressure ulcers
Good pressure care needs to be practised across all activities of daily living: in the wheelchair, in bed, in the bath and on the toilet or commode. Correct pressure care equipment is an important component of any prevention programme, but should not be seen as a complete solution.
A prevention programme for people at risk of pressure ulcers may include the following:
Correct positioning in bed or chair
People at risk of developing pressure ulcers should be repositioned throughout the day. When lying in bed, a 30 degree tilt will minimise pressure on bony prominences. Using a knee break and removing any slings or slide sheets will also protect from shear and friction. Consideration must be taken when placing someone in this position as it may not be suitable for everyone, for example, people with fractured hip joints or those with other complex conditions. Therefore, professional advice should be sought as part of developing a person’s care plan for managing their pressure ulcers (Wilson 2008).
When sitting in a chair, the chair needs to support the full length of the user’s thighs and keep the hips, knees and ankles at right angles. Armrests are required for user repositioning and transfers.
Changing position or lifting the body
Pressure should be relieved from any part of the body at regular intervals – especially over bony prominences. Areas at risk include:
- when lying on the back: shoulder blades, elbows, back of the head, buttocks and heels
- when lying on the side: shoulder, ear, hips, thighs and ankles
- when sitting in a chair: buttocks, elbows and heels.
Removing pressure completely allows time for the blood to flow normally to that area so that skin cell oxygen levels can be restored. If a person cannot change positions independently, he/she will need to be repositioned or moved by a carer. It is important to use correct manual handling techniques when repositioning. The intervals at which repositioning should occur depends on the person’s level of risk. A general rule is to change position at least once every 15 to 30 minutes (NHS Choices 2017).
A turning chart or clock may assist carers to establish an effective turning regime.
Regular inspection of the skin
An initial inspection of a new patient or client should occur immediately when a new care team is in place (or if admitted to hospital). A standardised assessment such as the Waterlow scale should be used for this initial assessment.
The skin should then be inspected frequently – depending on the person’s level of risk. Areas of risk should be inspected for:
- persistent redness which does not disappear after removal of pressure
- discoloration or a change in texture of the skin
- warmth or swelling over a bony prominence
- breaks, blisters or abrasions to the skin.
If a person is examining him or herself, a long handled mirror may be used.
Wearing suitable clothing and using suitable bedding
Sitting or lying on thick clothing seams, such as those in jeans, should be avoided as this can contribute to pressure ulcers.
Bedding should be free from wrinkles and a bed cradle may be used to decrease the pressure of bedding through the heels. Plastic or rubber backed bedding may cause an increase in moisture. Ideally, sheets and cushion covers should be two-way stretch and vapour permeable.
Good diet and healthy habits
A healthy and varied diet can reduce the risk of skin damage through ensuring you are getting adequate nutrition, and can also assist in helping with the healing process if you already have pressure ulcers. If you smoke, it may be wise to consider cutting down the amount you smoke or stopping smoking altogether. This is because smoking can reduce the level of oxygen in your blood and can weaken your immune system – both these factors increase the risk of developing pressure ulcers (NHS 2017).
Taking care when lifting and transferring
To reduce the effect of friction and shear on the skin, appropriate manual handling techniques and equipment need to be used. Slide sheets and hoists can be useful to reduce shear when transferring or repositioning although they should not be left underneath the user.
Using barrier creams
Some creams and oils may be recommended as a preventative measure, or to aid in healing of an existing ulcer. It is important to seek medical advice prior to use.
When washing and drying, the skin should be treated with care, especially in at risk areas. Talcum powder should not be used as this can dry out the skin and may cake and increase friction.
Using pressure relief equipment
Pressure relief equipment may include cushions, mattresses, bed cradles and joint protectors. Some products may have a pressure relief rating to assist health professionals to choose the correct pressure relieving products for their client. These ratings have been provided by the product’s suppliers, and are designed to provide a guide as to the pressure relieving qualities of that product. The ratings are intended as a guide only and consultation with your health professional and the product supplier before purchasing any equipment is strongly advised.
Properties and features of pressure relief mattresses and cushions
Pressure relief products distribute pressure in a variety of ways, including:
- conformity
- moisture absorption
- reduction of shear.

Factors to consider when choosing appropriate pressure relief include the following.
Conformity
Products made of water, air, gel and memory foam move and conform to the shape and movement of the body. However, these products decrease the ability to relieve pressure by leaning to one side as the surface will move with the user.
Stability
The user who finds it difficult to maintain sitting balance may find that cushions that conform quickly to the body and move do not feel particularly safe. They can also make transferring on and off the surface more difficult. If the user needs to push down on a transfer surface to gain leverage, the contents will move as soon as the body weight is lifted and the support will disappear.
Bottoming-out
If a mattress or cushion is too soft or thin, it may become compressed, allowing the skin to come into contact with the surface beneath, thus removing any pressure relieving qualities. This is called bottoming out. Turning cushions and mattresses may help to prevent this.
Shear forces
Some mattresses and cushions are designed to reduce shear forces as much as possible. Mattresses and cushions which have individual balloon or egg-box-shaped surfaces, or foam mattresses and cushions which have a cross cut surface are able to move with the body so that the pull on the outer layer of skin is decreased. Also, cushions which are ramped and slope backwards decrease the likelihood of users sliding forward in the chair thereby minimising shear.
Heat
As heat increases so does the risk of developing ulcers. Users who tend to get hot and sweaty may prefer to use a cushion that keeps the surface temperature of the skin cool. Water and gel help to conduct heat away from the area. Gel may be too cold for some people. Too much cold may cause the metabolism of the cells forming the skin cells to slow down so that they absorb much needed oxygen more slowly.
Standard foam mattresses and cushions and bead-filled mattresses and cushions should be avoided by people who get too hot, as they retain heat and do not let air circulate. Conversely, this type of mattress or cushion may be suitable for people who feel the cold and need their mattress cushion to act as insulation.
Moisture absorption
The amount of moisture produced may relate to the amount of heat produced and so may be influenced by the factors mentioned above. Moisture absorption also tends to be influenced by the material from which the mattress or cushion cover is made. Covers made of cotton and towelling are absorbent. Vapour permeable materials - for example platilon - allow the air and water vapour to circulate so that sweating is minimised. However, they are also water resistant so that if large amounts of fluid are spilt on it, the cushion underneath stays dry. Natural sheepskins are able to hold a high level of water vapour without feeling wet and will therefore reduce the effect of sweating. Man-made materials, such as nylon and vinyl, are not absorbent and, because they do not allow the air to circulate, may cause excess sweating.
Fire retardancy
Pressure relief cushions and mattresses are tested to criteria set by the Medicines & Healthcare products Regulatory Agency (MHRA). Also consider standards set by the British Standards Institute (BSI) on fire retardancy; these are very important, especially for users who smoke and/or those who are unable to get themselves out of bed or a wheelchair in an emergency.
Waterproofing
A user with continence problems should seek help from a continence adviser as to how these can be managed or prevented. Occasional accidents may be unavoidable. So, if the mattress or cushion is likely to be damaged if it gets wet, adequate waterproofing should be provided. A material such as platilon may be used as it is both waterproof and water permeable, i.e. moist air can circulate through it.
Cleaning
Check whether the mattress, cushion and/or the cover are washable and if they can be disinfected if necessary. A platilon cover can be wiped clean, thus avoiding the need to launder the contents.
Maintenance
The adjustment of some mattresses and cushions requires a certain amount of dexterity initially so that the correct amount of pressure relief is provided. The means of adjustment may make it necessary for someone other than the user to check and make the adjustments. Some mattresses and cushions have power packs that could go wrong; others may need mending after a puncture or a split. In the case of a wheelchair cushion, check whether the user can carry out these checks and/or repairs, or has a carer who could help. If there is no one available to help, it may be better to choose a cushion that does not need setting up and maintaining in this way.
Weight
The portability of the cushion will be important for those users who frequently need to lift it in and out of their wheelchair or car. Some cushion materials, like gel or water, are heavy and are not easy to lift even when there are handles on the cushion.
Cost
Mattresses and cushions vary widely in price. However, expensive ones may be cost effective in the long run and better for the wellbeing of the person if they prevent ulcers from forming and the user from being admitted to hospital for treatment.
Types of material used in mattresses, overlays and cushions
Air alternating cushions, mattresses and overlays

These are made of rows of air cells which inflate and deflate alternately or sequentially for a pre-set time period. This ensures that the pressure on any given point is changing continually, so that the pressure is completely removed from that point for a short period of time. Consequently, pressure is then increased over the other areas. Care must be taken to ensure that the user can tolerate these pressures.
The sequence of inflation and deflation is controlled by a pump which is usually mains powered. The interval of inflation and deflation can also be controlled on some models.
As with the static air cushions, they are unlikely to provide a stable base, and users may therefore need to consider their method of transfer.
Static air cushions, mattresses and overlays
The pressure relieving properties of these cushions and overlays relies on the fact that they are air filled.

Regular maintenance is required to ensure the correct degree of inflation is maintained. It is essential to check the instructions as it is sometimes easy to over or under inflate.
Air is channelled within these cushions via air-filled balloons or pathways. The balloon type increases the surface area over which the pressure is distributed. The pathways help the air to circulate and to disperse the heat and moisture.
It should be remembered that air is unlikely to form a stable base and users may therefore need to consider their method of transfer.
Foam cushions, mattresses, overlays
Single or varied density
The pressure relieving qualities of foam depend on its resilience. Foam cushions come in a variety of thicknesses, sizes and densities. Sometimes a cushion will be made up of a variety of different foam densities. The variations make allowances for differences in the weight of a user.
Foam deteriorates if exposed to heat or ultra violet light and should be checked regularly, with consideration given to replacing it every six to nine months depending on wear and usage.
To prolong the life expectancy and pressure relieving properties of a foam mattress/cushion it should be turned regularly, on a weekly basis. A high density foam base can make the cushion last longer.
Foam cushions tend to be lightweight and need no adjustments or maintenance; some can be cut and sculpted to order.
Cross cut, contoured, convoluted
 Cross cut, contoured and convoluted foam allows greater conformity and can reduce friction and shear by allowing the surface to move with the user. They also provide greater ventilation for the skin than other foams, as flat surfaced foam can act as an insulator and increase skin temperature.
Cross cut, contoured and convoluted foam allows greater conformity and can reduce friction and shear by allowing the surface to move with the user. They also provide greater ventilation for the skin than other foams, as flat surfaced foam can act as an insulator and increase skin temperature.
Memory foam
Heat sensitive or conforming foam with slow memory release models the shape of the body better than standard foam. The slower conforming properties of this material may enhance stability.
Gel cushions, mattresses, overlays
 Gel cushions work on the principle that the weight of the user is distributed over the liquid or solid gel. The gel is able to conform to the body shape, so that the pressure is distributed over the whole area.
Gel cushions work on the principle that the weight of the user is distributed over the liquid or solid gel. The gel is able to conform to the body shape, so that the pressure is distributed over the whole area.
Gel is able to conduct heat away from the user so that the cushion is cool to sit on. Liquid gel cushions will leak when punctured and gel cushions can be very heavy unless they are combined with another, lighter material.
Care needs to be taken in relation to transfers since gel alone is unlikely to form a stable seating base. Users may therefore need to consider their method of transfer.
Water cushions, mattresses, overlays
Water cushions can be less stable than gel (although more stable than air) and so do not provide much postural support. They are heavy to move and, if punctured, the rapid loss of contents may cause a problem. They are not stable, especially when the user is transferring, unless the flow of water can be reduced by enclosing it in multiple compartments.
Combination filling cushions, mattresses, overlays
 Cushions, mattresses and overlays that contain a combination of pressure relieving materials are usually arranged to provide a degree of stability to the seating base.
Cushions, mattresses and overlays that contain a combination of pressure relieving materials are usually arranged to provide a degree of stability to the seating base.
The combination of different materials may have the advantage of being lighter than one material on its own.
These cushions must be positioned correctly to achieve optimum pressure relief. A cover with a positioning guide, for example “this way up” or “this end to the back” may help to ensure correct use.
Air and liquid
Air and liquid cushions have a compartment for air surrounded by small water-filled cells. When inflated, the support comes from the air compartments. The water provides a cool surface to sit on.
Gel cushions with a foam base
These cushions have a foam base with a gel pad on top. The foam allows for a greater degree of stability than gel alone. Also, given that the amount of gel in the cushion is small, they tend to be significantly lighter than gel alone.
Water and foam
Water and foam cushions are made of open foam filled with water. The foam not only helps to add stability but also helps the cushion to conform to the body shape. They are cold to sit on and can therefore reduce skin temperature. However, remember that the foam will still deteriorate so that these cushions have quite a short life span.
Cushions with aperture
These cushions may be made of water, gel, memory foam or any combination of the above. They are designed to provide relief on a commode, toilet or bath hoist seat.
Advice for people who need pressure relief whilst sitting in an armchair
Chairs with integral pressure relief cushions
The integral pressure relief cushioning on these chairs is either on the seat base only or on the seat base and backrest. This is an alternative to adding pressure relief cushions to an existing armchair. Adding extra cushions changes the seat height and reduces the height of the armrests or reduces the depth of the chair. The position of the user is not compromised in a chair with integral pressure relief and there is less risk that the cushion will be the incorrect size, wrongly positioned or will slip.
Using pressure relief cushions in armchairs
Most pressure relief cushions are designed to work best when placed on a firm, level seat. When placed on a soft chair cushion they will lose some of their pressure relieving properties, as a person changes position in relation to the backrests and armrest height. Altering the surface of the armchair may also affect the ability of a user to get in and out of the chair.
Types of beds with pressure relieving features
Lateral tilting beds and devices
Lateral tilting beds
These beds turn the user from side to side, eliminating the need for turning by carers. They provide pressure relief and can assist in postural drainage, that is, drainage of fluid or mucus from the lungs. Turning can be programmed or transfer facilitated.
Lateral tilting turning units
These units can be used on top of a domestic bed. A longitudinally sectioned mattress is alternately inflated and deflated, which has the effect of tilting the person from side to side.
The units can be controlled by the person or the carer using a handset or can be set to automatically turn at pre-programmed intervals.
Low air loss beds and mattresses
These beds and mattresses have air sacs that support the user on a cushion of air. They work by increasing the surface area in contact with the skin, therefore reducing the pressure at a particular point. Air is gradually lost and continually replaced in response to the weight distribution and movement of the user.
They can be used with or without a cover or sheet; however plastic and rubber backed sheets should not be used as they prevent air flow.
Some of these beds are not solid enough for emergency resuscitation to be effective (CPR), so they may be supplied with emergency valves to deflate the mattress rapidly in an emergency.
Fluidisation beds
These beds are used mostly in hospital or care home settings rather than in the home. They are bath shaped. The pressure relief they provide is the result of pumping a large volume of air through a mass of particles - for example silicone beads - to make the particles behave as a fluid. When the air pump is stopped the beads become solid and support the user for nursing purposes. A hoist may be needed for transfers on and off these beds.
Water beds
These beds are mostly for hospital or care home settings rather than domestic use. They have a fluid interior which may have a foam perimeter helping to provide stability. The fluid is cold to lie on; they can therefore reduce skin temperature. However, the fluid makes the beds very heavy and care must be taken as to where they are sited. Since it is difficult to transfer safely from a moving base, using a hoist is recommended.
Joint protectors
Some people need to use joint protectors for comfort, protection and pressure relief. These may come in the form of a pad which is tied around the elbow or heel or in the form of a bootee which encloses the toes. However, ensure that the fastenings do not exert pressure. They come in a variety of pressure relieving materials. The following types are available:
- fleece joint protectors
- fleece bootee joint protectors
- polyester fibre joint protectors
- air filled or fluid filled joint protectors
- foam joint protectors
- pads for walking equipment and prostheses, for example to line the socket of a prosthetic limb to protect the skin.
Supply and provision
Permanent loan: health and local authority provision
Wheelchair cushions
The provision of wheelchair cushions is carried out by, or through, the wheelchair service. This is part of the health authority and organised on a district-wide basis. These services are able to provide a wide range of wheelchairs and cushions. A pressure relief cushion needs to be prescribed at the same time as the wheelchair to ensure that it does not affect the functional ability of the user. If the cushion is too high, it may prevent users from reaching the propelling wheels or make it difficult for them to get their legs under standard height tables.
Referral
A Referral to the wheelchair service can be made by a range of professionals including therapists, nurses and doctors.
Range of equipment available
Standard off-the-shelf cushions and individualised made-to-measure cushions are available. Assessment and authorisation for these cushions needs to be carried out by various health professionals including an occupational therapist and physiotherapist.
Home nursing equipment
Home nursing equipment such as pressure relief mattresses and armchair cushions may be supplied by a District Nurse or Community Matron. He/she can usually be contacted through the local health authority or via your GP. Manual handling training and equipment such as hoists are usually provided by an occupational therapist in the community.
Referral
Referrals to community nurses and occupational therapists can be made by a range of health professionals including doctors, other nurses and therapists.
Range of equipment available
A range of pressure relieving mattresses, cushions and beds may be available as well as manual handling equipment such as hoists and slide sheets.
Employment service
Employment equipment and adaptations are defined as any equipment which is primarily for the purpose of meeting an employment need. This could include wheelchairs and cushions, ramps, short rise lifts and stairlifts.
Employment equipment and adaptations are provided through:
- The Disability Services Teams (DSTs) part of Universal jobmatch
- Work coaches who work from local job centres and who, as well as providing a wide range of advice and help to people who have particular difficulties in finding or keeping work because of a disability, can also advise on how to obtain equipment.
Purchase of equipment
Private purchase
Private purchase might be preferred either because a person wishes to buy privately, or because the statutory services are unable to provide the item required.
Funding from charitable sources
Charitable trusts may sometimes provide funding for equipment. A useful resource is Turn2Us, a website that allows you to search for organisations that give grants, including equipment and other services. You can refine your search by specific conditions - visit their website and search for grant giving organisations using their filter categories (e.g. mental health, older people, musculoskeletal disorders) such as help with debt relief or the Florence Nightingale Aid-in-Sickness Trust.
Charities will only give awards in accordance with a predetermined criteria, so it is important that you carefully select the trusts you apply to.
Most libraries hold directories of suitable funders in their reference section, such as the Directory of Grant Making Trusts. The Grants for Individuals website is run by the Directory of Social Change and lets subscribers search for grants but is intended for organisations searching for funding for individuals.
Selecting appropriate equipment
If you decide to purchase pressure relieving equipment privately, try and compare the different ranges first, perhaps in your local Independent Living Centre. They provide unbiased, expert advice and information about equipment, how much it costs and where to obtain it. They also offer the opportunity for you to try a wide range of products.
Advice and information about other issues related to daily living is also available.
It is always advisable to contact the centre before visiting to check whether you need to book an appointment, and to also check for up to date opening hours which may be subject to change.
Be cautious of sales people who try to persuade you to buy equipment that may not meet your needs fully or is over-priced. Buying from a company that belongs to a trade association, such as the British Healthcare Trades Association (BHTA) may give you some reassurance. BHTA members have signed up to a code of practice governing standards of customer service (see Useful organisations below).
VAT relief
You don't have to pay VAT on products designed for disabled people if you have a long term illness or disability, or are terminally ill.
Mobility shops may automatically sell you equipment without charging you VAT, but you may have to ask for this to be discounted off the total price.
Individuals with a temporary injury such as a broken arm or hip do not qualify for VAT relief.
For more information, and to check for any changes in the regulations visit:
- GOV.UK's website: VAT relief on products and services for disabled people
- GOV.UK's information on reduced rate VAT. Their Charities Helpline covers VAT relief for disabled people. Call 0300 123 1073.
Further advice from us
For clear, practical advice and information on products and suppliers of daily living equipment, please have a look at our Living made easy website.
If you would like further advice related to choosing equipment for everyday living you could try relevant sections of AskSARA, our free online guided advice tool. AskSARA will ask you questions about yourself and your environment and then offer relevant advice, product suggestions and supplier details.
You can contact the DLF Helpline, which is open Monday to Friday from 10am to 4pm. Tel: 0300 999 0004 (calls charged at your standard land line rate even if you are phoning from a mobile).
Alternatively, you may wish to contact us via email: info@dlf.org.uk or by letter: DLF, 34 Chatfield Road, Wandsworth, London SW11 3SE
To help us give you a concise and informative reply, please provide us with as much detail as possible, including information on the difficulties you are having and any solutions you have considered, such as equipment ideas.
Another source of advice is a disabled or independent living centre where you would have the opportunity to try out a range of equipment. There are several of these around the country where you can go for impartial advice. Your local authority will also be able to give you details of centres in your area.
Useful organisations
7 The Court, Holywell Business Park, Northfield Road, Southam, Warwickshire CV47 0FS
Tel: 01926 357220
Email: help@bladderandbowel.org
Website: www.bladderandbowel.org
The Bladder and Bowel Community was created to support millions of people who are living with conditions that affect their bladder or bowel. They provide an online community and access to essential information and guidance on specific bladder and bowel conditions and treatments.
Disabled Living, Burrows House, 10 Priestley Road, Wardley Industrial Estate, Worsley, Manchester M28 2LY
Tel: 0161 607 8219
Email: bladderandboweluk@disabledliving.co.uk
Website: www.bladderandboweluk.co.uk
Bladder and Bowel UK have a team of dedicated specialist nurses and knowledgeable continence product information staff who provide information about continence and bowel problems for children, young adults, and adults. They also have a wide range of training and education resources for health professionals.
Suite 4.06 The Loom, 14 Gowers Walk, London, E1 8PY
Tel: 020 7702 2141
Email: info@bhta.com
Website: www.bhta.net
The BHTA is the UK's largest healthcare association. Members of the BHTA sign up to a code of practice designed to ensure the public can trust that members will give a good service, and a high standard of behaviour.
C/O Codan Consulting, Provaznicka 11,110 00, Prague 1
Tel: +420 251 019 379
Email: office@epuap.org
Website: www.epuap.org
The European Pressure Ulcer Advisory Panel aim to provide relief for people suffering from, or at risk of, pressure ulcers, through research and the education of the public and by influencing pressure ulcer policy in all European countries towards an adequate patient centred and cost effective pressure ulcer care.
151 Buckingham Palace Road, Victoria, London SW1W 9SZ
Tel: 020 3080 6000
Email: info@mhra.gsi.gov.uk
Website: www.mhra.gov.uk
The MHRA regulate medicines, medical devices and blood components for transfusion in the UK. The MHRA is an executive agency, sponsored by the Department of Health.
High Corn Mill, Chapel Hill, Skipton, North Yorkshire BD23 1NL
Tel: 01756 799950
Email: info@bedfed.org.uk
Website: www.bedfed.org.uk
The National Bed Federation is the recognised trade association representing UK manufacturers of beds and their suppliers. Founded in 1912, members account for about 75% of the total UK bedding turnover.
20, Cavendish Square, London W1G 0RN
Tel: 020 7409 3333
Website: www.rcn.org.uk
The RCN is a membership organisation of over 435,000 registered nurses, midwives, health care assistants and nursing students. The organisation offers representation of the professional interests of nursing staff working in the public, private and voluntary sectors, support to members in respect to confidential advice on employment matters, career development, immigration, welfare and more and they influence and lobby the Government and other bodies across the UK, to develop and implement policy that improves the quality of patient care.
Cherry Hill, South End, Roos, East Riding of Yorkshire HU12 0HJ
Tel: 0845 527 6651
Email: tvs@tvs.org.uk
Website: www.tvs.org.uk
The TVS works in partnerships with its members on a range of initiatives including establishing and supporting a new wounds research network, emphasising multidisciplinary working and introducing members to the latest research and knowledge.
Released August 2017, to be reviewed by August 2020, Version 1
References and further reading Show references
References and bibliography
NHS Choices (2017) Pressure Ulcers – Symptoms [Online] Available at www.nhs.uk/Conditions/Pressure-ulcers/Pages/Introduction.aspx [Accessed 9 June 2017] - Type 2
Wilson, M (2008) Repositioning Patients to Prevent Pressure Ulcer Formation: The 30 degree Tilt. Wound Essentials Vol 3 pp.100-101 – Type 2
For more information on the Types of Evidence, please visit http://www.livingmadeeasy.org.uk/scenario.php?csid=276
| Attachment | Size |
|---|---|
| 2.23 KB | |
| 9.54 KB | |
| 6.95 KB | |
| 5.34 KB | |
| 13.45 KB | |
| 10.97 KB | |
| 5.15 KB | |
| 10.5 KB | |
| 38.79 KB | |
| 99.85 KB | |
| 30.25 KB | |
| 96.3 KB | |
| 76.12 KB | |
| 21.99 KB | |
| 6.94 KB | |
| 12.15 KB | |
| 6.17 KB | |
| 85.49 KB | |
| 11.06 KB | |
| 428.15 KB |
All rights reserved. No reproduction or transmission of this publication may be made without written permission. Inclusion (including any sponsorship) does not indicate endorsement or that any item has been recommended or tested. All information is provided without legal responsibility.
Disabled Living Foundation, Tel: 020 7289 6111, Fax: 020 7266 2922, Helpline: 0300 999 0004 10.00am-4.00pm, Email: helpline@dlf.org.uk, Website: www.dlf.org.uk
Reg. Charity No: 290069, VAT Reg. No: 226 9253 54
 (Tell me about the standard)
(Tell me about the standard)
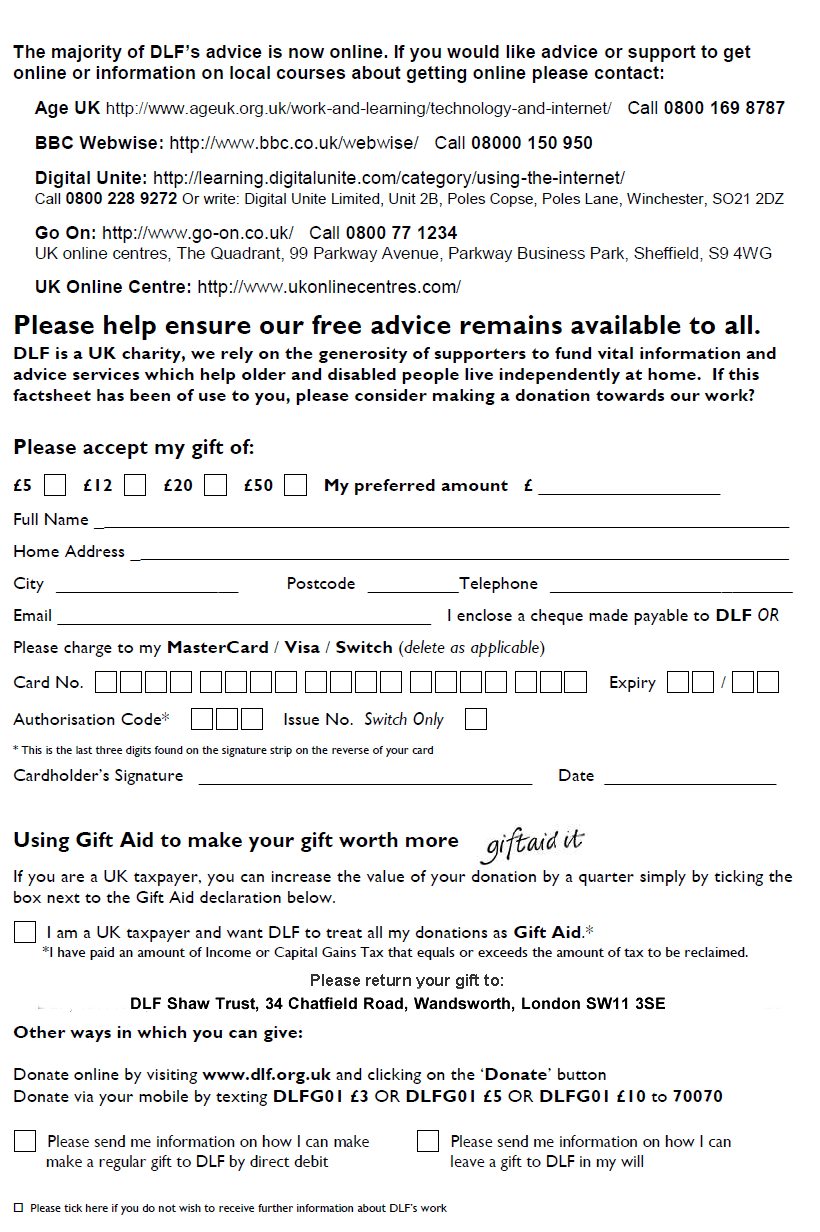
Your personal information is required in order to claim Gift Aid. This information is kept by DLF/Shaw Trust for financial audit purposes. For more information on our privacy policy visit: https://www.dlf.org.uk/content/privacy-policy








